Blood Group Genetics

CURRICULUM ALIGNMENT
- Frequencies of genotypes and phenotypes of offspring can be predicted using probability models, including Punnett squares, and by taking into consideration patterns of inheritance, including the effects of dominant, autosomal and sexlinked alleles and multiple alleles, and polygenic inheritance (ACSBL085)
BACKGROUND
Blood Types: The fundamental function and composition of blood is the same in everybody. However, there are several blood types within the human population, and they are not compatible with one another when it comes to blood transfusions. This variation in blood types results from differences in red blood cell surface molecules. Like other cells, there are molecules that project from the surface of the cell membrane of red blood cells. Some select sugar and protein molecules on the surface of the cell act as identification markers that indicate the cell is a normal part of the body; and therefore, the immune system knows not to attack it. If blood from an individual with different surface molecules is transfused into another, the immune system recognises it as antigenic (foreign to the body) and therefore attacks the Antigens in an attempt and the cells that carry them. To combat this, donated blood is tested for A, B, O, and Rh Antigens, so that blood is only transfused into compatible recipients.
The ABO Blood Groups: The presence or absence of two Antigens, A and B, on the surface of the red blood cells result in the ABO blood groups (types). The immune system recognises Antigens that are present very early in life as a normal part of the human body, and therefore does not develop an immune response to them. Antigens are inherited from the parents’ genes. Without an immune response, antibodies to any A and B Antigens present in the blood cells are not developed in the body. However, A and B blood Antigens not present on the organism’s own cells will cause the immune system to produce antibodies. In blood Type A, the A antigen is present on its red blood cells and anti-B antibodies are present in the Plasma. In blood Type B, the B antigen is present on its red blood cells and A antibodies are present in the Plasma. Type AB blood contains both A and B Antigens on the red blood cells and no antibodies are present in the Plasma. Type O blood contains neither A or B Antigens on the red blood cells and both A and B antibodies are present in the Plasma. These antibodies will be present, regardless of whether the person has had foreign blood introduced into their body. The antibodies are believed to be present due to the similarity between A and B blood Antigens and common Antigens we encounter in the environment. Antibodies generated for one antigen will recognise another if the two Antigens are very similar. Type O blood contains neither A or B Antigens on the red blood cells and both A and B antibodies are present in the Plasma. These antibodies will be present, regardless of whether the person has had foreign blood introduced into their body.The antibodies are believed to be present due to the similarity between A and B blood Antigens and common Antigens we encounter in the environment. Antibodies generated for one antigen will recognise another if the two Antigens are very similar.

Using Agglutination to Determine the Blood Type: Agglutination describes the clumping of particles and results from an antigen being mixed with its corresponding antibody. For example, agglutination will occur in a blood test if blood type A interacts with Anti-A antibody serum.
Using Agglutination to Determine the Blood Type: Agglutination describes the clumping of particles and results from an antigen being mixed with its corresponding antibody. For example, agglutination will occur in a blood test if blood type A interacts with Anti-A antibody serum.
Using Agglutination to Determine the Blood Type: Agglutination describes the clumping of particles and results from an antigen being mixed with its corresponding antibody. For example, agglutination will occur in a blood test if blood type A interacts with Anti-A antibody serum.
Investigation scenario
You are a blood geneticist working for a medical laboratory. You have received an unusual request from a couple named John and Andrea Dean. John and Andrea Dean are a wealthy couple who live with their daughter Sally in Sydney. One day they are having a nice family BBQ when a young man shows up at the door. He introduces himself as Michael and claims to be Andrea’s son. He claims that Andrea had a son at the age of 16 whilst in high school and put him up for adoption. Michael says how excited he is to meet his real mother but an embarrassed Andrea strongly denies his claims. Andrea says Michael is a liar who is clearly after their money. John is not sure what to think as Michael seems so genuine and suggests the entire family take a blood test to be sure. And that’s where you come in. John and Andrea Dean have enlisted your help to determine if Michael is Andrea’s biological son. Using Agglutination you will determine the blood type of John, Andrea, Sally and Michael.
METHOD - STUDENT ACTIVITY
- Allocate 1 pipette for each Anti Sera and genetic blood sample. Label each pipette bulb accordingly using a permanent marker. Allocate and label 1 well plate for each blood sample to be tested.
- Using the appropriate pipette, transfer a drop of John’s blood sample to each well of the blood typing slide. Replace the cap on the vial to prevent cross contamination between different samples.
- Transfer a drop of synthetic anti-A (blue) to the well labelled A.
- Transfer a drop of synthetic anti-B serum (yellow) to the well labelled B.
- Using a mixing stick, carefully mix the synthetic blood and antibody serums for 30 seconds. Use a different mixing stick for each sample to avoid cross contamination. Use a blue mixing stick for anti-A, yellow for anti-B. The sticks are single use only.
- Once all the serums have been mixed into the synthetic blood sample, examine the samples in each well and look for the presence or absence of agglutination. If the liquid has a uniform texture, no agglutination has taken place. A granular sample will indicate that agglutination has taken place.
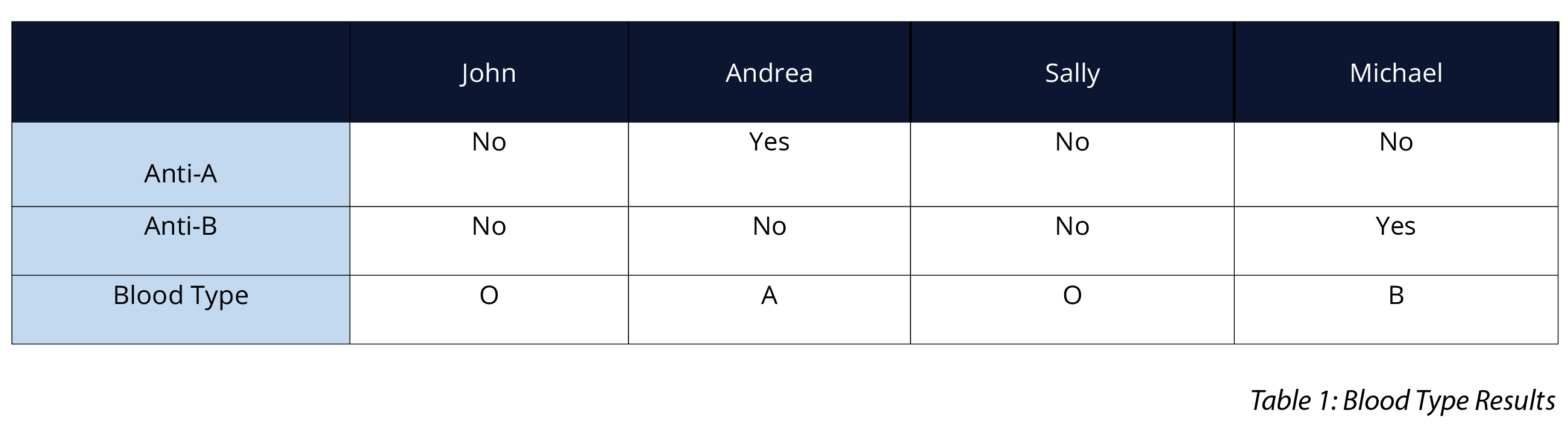
- Record the results in Table 1. Simply write ‘yes’ or ‘no’ as to whether agglutination occurred with each antibody serum. A positive agglutination reaction indicates the blood type. Determine and record John's blood type in Table 1.
- Repeat the same procedure (steps 2-7) using Andrea, Sally's, and Michael’s blood samples.
OBSERVATION AND RESULTS
Below is the expected results for this experiment.
INVESTIGATIONS
- Based on these results, ask students what John and Sally's genotype are. Students should identify that both John and Sally's genotypes are O, indicating they are related.
- Based on Andrea's blood type, along with John and Sally's genotypes, challenge students to find Andrea's genotype. Students should identify that Andrea's genotype is AO.
- Ask students to fill in a Punnett square showing the possible genotypes for John and Andrea's children. Their Punnet square should look like the example below.
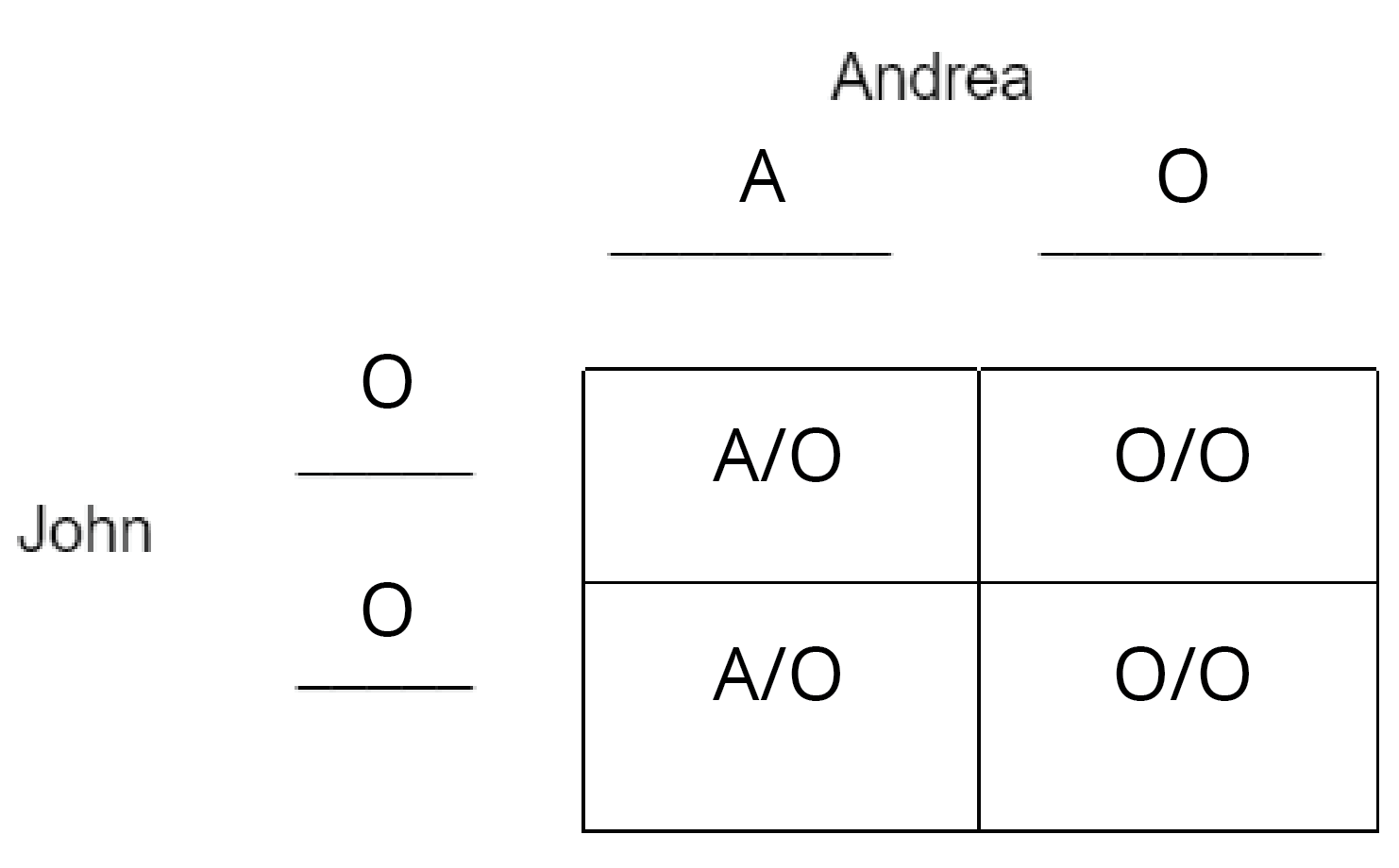
- Using the Punnett square, ask students what the possible blood types (phenotypes) of John and Andrea's children are. Students should identify that John and Andrea's children will have either A or O blood types.
- Based on the results of the blood testing ask students whether is it possible that Michael is the son of John and Andrea Dean.
 Time Requirements
Time Requirements
- 45 mins
 Material List
Material List
- 1 Vial Synthetic Anti Sera A
- 1 Vial Synthetic Anti Sera B
- 4 Vials Synthetic Genetic Bloods
- 4 Blue Mixing Sticks
- 4 Yellow Mixing Sticks
- 4 Blood Tiles
- 6 Plastic pipettes
- Paper Towels
- Access to Tap Water and a Sink
 Safety Requirements
Safety Requirements
-
Wear appropriate personal protective equipment (PPE).
- Know and follow all regulatory guidelines for the disposal of laboratory wastes.
